
SMART BANDAGES SAVE LIVES
Soldiers receive remote treatment via electronic wound dressing
- Dateline
- 5 April 2013
Denis Moore is awake and, more importantly, both his legs are still attached to his body. Moore was in a remote part of Afghanistan, serving with British forces, when he accidentally tripped an improvised explosive device.
Paramedics did what they could and then bound his wounded legs with a new experimental bandage. “The bandages are electronic, using the new Planar printed lithium-batteries. They’re about 3mm thick, flexible and can power the telemedicine electronics for around 10 hours,” says Sergeant John Chapman, the paramedic who treated Moore.
The printed batteries make them light and cheap, and have also opened up tremendous innovation in new devices. For the first time, things as thin and flexible as clothing can have fully active powered systems.
“The value of this technology is that we could monitor Moore’s injuries in real time and even administer the most appropriate medication via the bandage to ensure optimal recovery,” says Doctor Sheila Simms at Selly Oak Hospital, Birmingham.
“The bandage sends us a real-time scan of tissue and bone damage, and releases targeted drug particles.”
The batteries are expected to have a tremendous impact on mobile phones and computers but for one brave soldier it has already had a life-changing effect.
ANALYSIS >> SYNTHESIS: How this scenario came to be
Background
Thin film electronic printing utilizes all forms of industrial printing, from ink-jet, to screen printing, to nano-imprint lithography.
Gravure printing has been used to produce solar cells, reaching up to 10,000 square meters per hour. Such printing can also be used to produce organic semiconductors and semiconductor/dielectric interfaces in transistors.
Developing these inks is complex. For printing, viscosity, surface tension and solid content must be tightly controlled. Cross-layer interactions such as wetting, adhesion, and solubility as well as post-deposition drying procedures affect the outcome. Additives often used in conventional printing inks are unavailable, because they often defeat electronic functionality.
There is already significant experience and development in mass-production of solid-state electronics using printing techniques. Producing batteries in this way is more about experimenting with the necessary ‘inks’ than in inventing a new industrial process.
2011: Paper-thin batteries meet smart bandages
Planar Energy, a spinoff of the US Department of Energy’s National Renewable Energy Laboratory, launches their first solid-state printed lithium battery. The company’s batteries store 400 watt-hours of energy per kilogram. “Our energy density is a factor of two or three higher than lithium-ion, and we can do that at about a third of the cost,” says Planar’s CEO, Scott Faris.
They’re followed closely by fellow US firm, Paper Battery, which is producing ultracapacitors capable of holding 10 to 15 watt-hours of energy per square meter. “If you are able to contact the full surface, you can get a very large amount of power,” says CEO, Shreefal Mehta. “The sheets can stand alone, but we see this as being integrated into another structure.” The company is co-developing a product with Philips’ medical diagnostic devices division.
Ultraportable medical diagnostics has long been held back by a lack of low-weight energy storage. That hasn’t stopped the development of a wide range of smart bandages. The University of Rochester in the US develops a sand-grain-sized silicon wafer that can differentiate between two classes of bacteria, Gram-positive and Gram-negative, and stains them different colors. Embedded in bandages, they permit rapid visual analysis of the nature of wound healing.
A similar project at the University of Bath aims to treat burns patients. Nanocapsules in the bandages release antibiotics to treat the wound and medics are alerted to the presence of harmful bacteria when the dressing changes color. “The dressing is only triggered by disease-causing bacteria, which produce toxins that break open capsules containing the antibiotics and dye. This means that antibiotics are only released when needed, which reduces the risk of the evolution of new antibiotic-resistant super-bugs such as MRSA,” says Project Leader Dr Toby Jenkins.
Researchers at the Holst Centre in Eindhoven, The Netherlands, are developing sensor films that combine light sources and photo sensors to measure the oxygen content of the blood that circulates within damaged tissue. “Embedded in bandages, these sensor films deliver important information about healing progress. Doctors are better able to determine the best time to change bandages and therefore speed up the healing process,” says Jaap Lombaers, Managing Director at Holst Centre.
And Shi Cheng and Zhigang Wu, at the University of Uppsala in Sweden, develop a self-contained large-area wireless strain sensor, operating at around 1.5 GHz, which permits the development of a smart bandage that can monitor the strain of a weakened joint, and provide feedback to a computer system that then presents healthcare warnings.
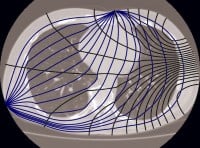
2012: Electrical impedance tomography shows promise
“Electrical Impedance Tomography is a harmless and inexpensive imaging modality. Unfortunately, it is known to be unstable, which makes it impossible to obtain high resolution images,” says Dr Leonid Kunyansky, from the University of Arizona.
However, in emergencies, even a low-resolution medical image can be of tremendous value. The process involves attaching conducting electrodes to the skin of the subject and applying small alternating currents to the electrodes. The resulting electrical potentials are measured, and the process may be repeated for numerous different configurations of applied current.
Students at Oxford Brookes University in the UK were developing three dimensional EIT images of chests for tracking lung-cancer when one student dropped a heavy piece of test equipment on his foot. “We were in the lab and waiting for the ambulance to arrive,” says Tiffany Roberts, a graduate student in the medical engineering department at Oxford Brookes. “John [Saunders, the student with the broken foot] was just sitting there, so I placed our test electrodes over his foot. It was amazing, the image wasn’t good – not as clear as an X-Ray – but you could clearly see the broken bones.”
With additional investment from Fujifilm – printed electronics manufacturers – and GE Healthcare – in medical imaging – Oxford Brookes starts investigating the opportunities in thin-film medical imaging devices.
2013: Smart bandages save lives
The potential for such combinations of devices in time-sensitive environments soon attracts the military. The Ministry of Defense Centre for Defense Enterprise invests a further US$ 25 million into Oxford Brookes.
“The biggest difficulty is ensuring that the electrodes don’t interfere with the bandage itself while still making a sufficient connection to ensure that we’ll see something,” says Dr Hugo Davies, at the MOD. But the basic components all exist and so, in a mere six months, the first smart bandages are ready for field-testing. And where better than in Afghanistan?
“At worst, it’s still a bandage. At best we get to treat casualties faster and more precisely than we ever thought possible,” says Dr Sheila Simms at Selly Oak Hospital, Birmingham.
In Afghanistan, Corporal Denis Moore is about to set off an improvised explosive device.
Links to related stories
- ‘Smart’ bandage to treat infectious wounds - UK Trade & Investment, 9 July 2010
- Wireless electronics take the strain - Richard Walters, Materials Views, 2 May 2011
- Printed Power Sources for Cars and Consumer Gadgets - Prachi Patel, IEEE Spectrum, 21 December 2010
- Electrical impedance tomography - Wikipedia
Warning: Hazardous thinking at work
Despite appearances to the contrary, Futureworld cannot and does not predict the future. Our Mindbullets scenarios are fictitious and designed purely to explore possible futures, challenge and stimulate strategic thinking. Use these at your own risk. Any reference to actual people, entities or events is entirely allegorical. Copyright Futureworld International Limited. Reproduction or distribution permitted only with recognition of Copyright and the inclusion of this disclaimer.